The cause of infertility will determine which treatment program you embark on. The type of program will affect your chances of pregnancy, as do a number of other factors including age and, if IVF occurs, the quality and number of the embryos replaced.
On average our pregnancy rates range from 15-50% per treatment cycle, depending on the type of treatment, unless a woman is above the age of 38 years, in which case they are lower.
This pregnancy rate may not seem as high as expected, but it is important to remember that humans are not particularly fertile as a species. If a couple with healthy fertility has intercourse at the time of ovulation, they still only have a 15-20% chance of having a pregnancy each monthly cycle.
The basic reason why many embryos fail to continue to grow has been investigated and researched for a number of years. Not all the reasons are yet understood, but genetic studies have indicated that shortly after fertilisation, a number of embryos contain significant errors in the information that they use to control their early growth and development. As a general rule, the number of embryos with errors increases with the increasing ages of the couple. IVF cannot change the quality of your eggs or sperm but attention to lifestyle factors can.
We include a regular review process in our treatment programs, so that if a treatment cycle is not successful, we assess the need to modify your next treatment cycle to improve your chances of success. If a pregnancy has not occurred, your specialist will review that treatment cycle to see if any changes need to be made and have a consultation with you to discuss future options if appropriate.

Not many people openly discuss the difficulties falling pregnant, and there is certainly a lack of awareness about female fertility in Australia. Most people have no idea how common fertility challenges are for women or how daunting it can be to overcome these obstacles.
The latest statistics show that:
Unlike other clinics, age is not a barrier at Fertility First. We have helped women up to 48 years of age have babies using their own eggs.
Use our calculator to determine the fertile time for different cycle lengths (14-19 days before next period).
A child’s gender cannot be influenced by the number of days before ovulation that intercourse occurs.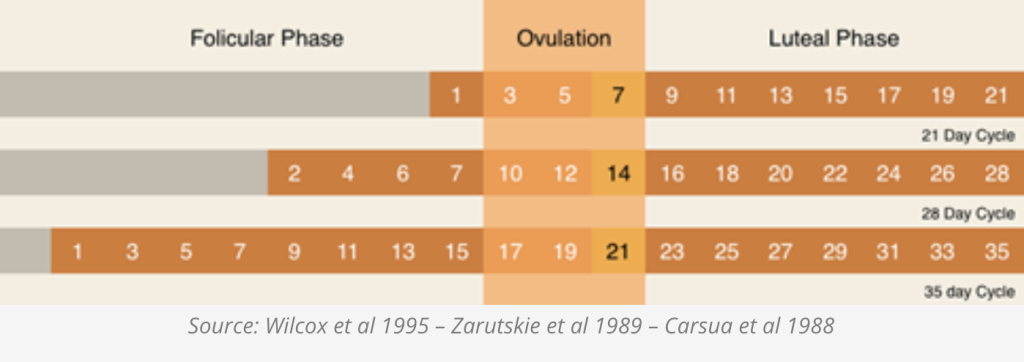
Also a topic that is rarely spoken about, male infertility accounts for up to 50% of all infertilities, and impacts approximately 7% of men.
Using donated sperm may be the best chance of achieving pregnancy for some couples. Each year about 4% of all children born in Australia are the result of Artificial Reproductive Technology, including Donor Insemination.
There are many natural options to improve your chances of falling pregnant. Through our individualised approach, we assess any lifestyle or environmental factors that may be affecting your infertility, and work with you to modify these if necessary. Factors such as Vitamin D, folate and iodine deficiency, insulin levels, weight, alcohol and smoking can all impact on the health of the sperm as well as the egg and therefore the chance of conceiving. They can also impact on the chance of staying pregnant and normal development of the baby.
Here are some general lifestyle changes that will help improve fertility in men and women.
The first consultation is always more thorough when both of you attend. To fit with your busy schedules, we offer a range of appointment day and times so you can find one that suits best.
To be eligible for Medicare rebates from your first visit, you need a current referral to Fertility First. GP referrals are valid for 12 months, and specialist referrals are valid for 3 months.
We believe it is important to investigate factors relating to your fertility problems as quickly as possible. To help minimise time of additional testing, we ask that not only both of you come to the first appointment, but we also have your history, examinations and blood tests completed. This will ensure the assessment process is as efficient as possible.
We aim to have your test results back within 2 to 3 weeks, which means, unless any assessment of the fallopian tubes is required, treatment options can then be considered.
If a semen analysis is required, it may be possible on the first appointment. There is a dedicated room set aside for this purpose. In order for us to conduct the analysis, you will need to make an appointment with the laboratory in advance so we have the right laboratory staff available to carry out the test. We prefer to combine the semen analysis with an assessment of sperm DNA damage, using the specialised Halosperm assay, as it is not possible to gain an accurate picture of a man’s fertility potential without this assay.
The semen sample can be collected at home, provided it can be brought in to the Fertility First laboratory within 45-60 minutes of collection.
If the woman’s fallopian tubes have not yet been assessed, we typically arrange that after the second visit, so another menstrual cycle may pass before all investigations are complete. The reason for waiting is that we believe that it is important to carry out all non-invasive investigations first.
For example, if there was a significant reduction in semen quality that meant in vitro fertilisation (IVF) was required, then an assessment of the fallopian tubes would not normally be necessary. Normal, open tubes are not required for IVF.
At Fertility First we aim to minimise the invasiveness of the testing process and only carry out those investigations that are required to maximise your chance of a successful outcome.
Unless IVF is being considered it is important to know if the fallopian tubes are open (patent) to decide what the best treatment options are.
Tubal assessment can be done via an ultrasound study called a hysterosalpingo-contrast-sonography (Hy-Co-Sy) or via an operation, called a laparoscopy, using “keyhole” surgical techniques.
We have information sheets on these procedures and the advantages and disadvantages of each one will be discussed with you. The surgery can be done by the medical staff at Fertility First, or your referring gynaecologist.
Don’t be one of those couples who spend years trying to fall pregnant before they seek help. If you’re planning to start a family – see us first, at Fertility First.